Key Takeaway:
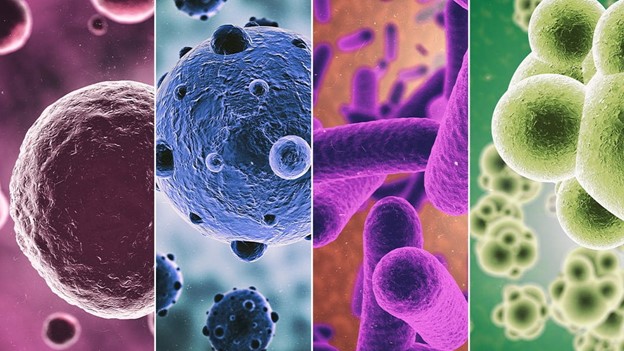
- Interactions between bacteria and viruses have the potential to worsen infections and potentially intensify secondary infections before they are diagnosed.
- An efficient management plan is necessary to control the infection because both viruses and bacteria were co-infected.
Modern technology has made it possible to identify the presence of bacteria and viruses in a variety of respiratory illnesses, including COVID-19, pneumonia, otitis media, and cystic fibrosis (CF). Studies have indicated that bacterial infections leading to subsequent pneumonia could have contributed to the 1918 pandemic’s high morbidity rate. Similar findings were made during the most recent COVID-19 pandemic, which showed that 68% of COVID-19 patients admitted to the intensive care unit (ICU) experienced secondary bacterial infections such as pneumonia, bacteremia, etc., which exacerbated the SARS-CoV-2 condition. The processes underlying the interactions and synergistic/cooperative relationship between bacteria and viruses in clinically important respiratory infections are reviewed in detail in this article.
The respiratory tract microbiota usually does not pose a threat to the body, and there is a balance between commensal and opportunistic pathogens and formal micro-flora. On the other hand, changes or dysbiosis in this community could lead to the acquisition of viral or bacterial pathogens and the transfer of opportunistic pathogens to pathogenic pathogens, ultimately causing pathogenic invasion. Both viruses and bacteria have been shown to facilitate viral infection and contribute to subsequent bacterial infection. Co-infection in CAP frequently makes the illness more severe and necessitates longer hospital stays. There have been suggestions that secondary pneumonia may have developed as the primary cause of death during the “Spanish Flu” pandemic. Like this, secondary pneumonia was responsible for 29–55% of deaths during the 2009 H1N1 pandemic. This was once more seen during the most recent worldwide COVID-19 epidemic, where the disease became more severe due to bacterial secondary infection.
The interaction between the virus and bacteria is intricate, and numerous factors, including the host’s immune system, the bacterium, and the virus, work together to predispose co-infections. Viral damage to respiratory epithelial cells, exposure of bacterial receptors, cilia damage, changes to the mucosal environment, immune system dysregulation, phagocyte function, promotion of the release of inflammatory mediators like chemokines, cytokine release, overexpression of antimicrobial peptides, and enhanced bacterial adherence are the mechanisms by which viruses can cause bacterial co-infection. Numerous research and observations have demonstrated that the interplay between bacteria and viruses can exacerbate illnesses and perhaps exacerbate secondary infections before diagnosis. Since bacteria and viruses co-infected, an effective management strategy is required to control the infection.
Reference: Lalbiaktluangi C et al. A cooperativity between virus and bacteria during respiratory infections. Front Microbiol. 2023; 14: 1279159.