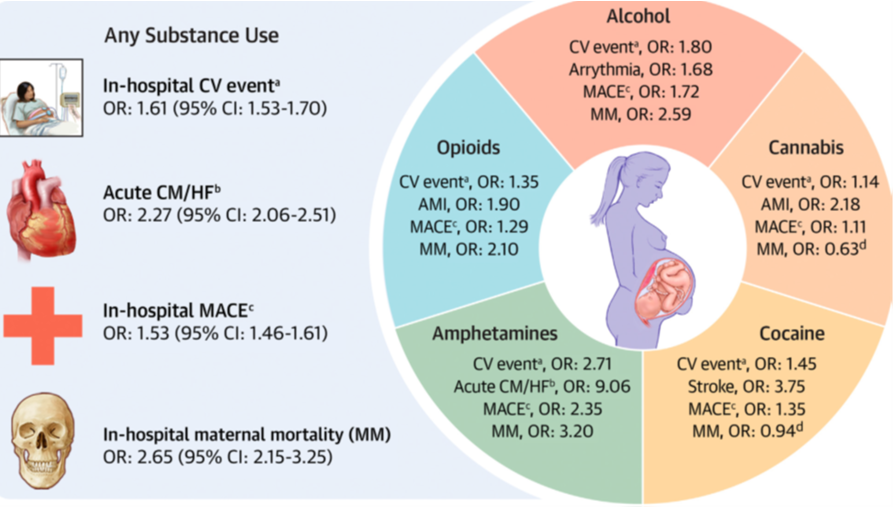
Key takeaway: Substance use is strongly linked to acute CV events and maternal mortality during labor and delivery, and women who use substances should be monitored more closely for CV events at this time.
The number of pregnant women who use drugs and have cardiovascular (CV) events is rising, but it is still unclear if substance use during pregnancy is related to CV events. A study hypothesized that substance use is associated with an increased risk of maternal CV events, which may contribute to increasing maternal morbidity and mortality. According to the study, the prevalence of any CV risk factor was highest.
amongst deliveries with substance use compared with deliveries without substance use (substance use: 53.1% vs no substance use: 13.0%; P < 0.0001). Also, the study showed that delivery hospitalizations with substance use were associated with a greater risk of any CV events after adjustment for age, race, traditional CV risk factors, and pre-existing medical conditions, compared to those without substance use.
With a 4-fold increase for deliveries including substance use and a 2-fold increase for deliveries avoiding substance use, the incidence of any CV event rose over time. Methamphetamine and amphetamine usage had a higher-than-average risk of experiencing a CV incident (P< 0.001). Every substance except amphetamine/methamphetamine, which was most frequently related to acute cardiomyopathy/heart failure, had an arrhythmia as the most frequent CV event at delivery hospitalization. Cocaine use showed the strongest link with stroke, alcohol use had the strongest association with arrhythmia (P <0.001), and opioid use had the strongest association with endocarditis (P<0.001). In conclusion, there is a significant correlation between acute CV events, substance use, and maternal mortality during labor and delivery. These findings have significant implications for maternal health as substance abuse among expectant women increases and maternal mortality rises.
Reference: Evans K et al. Substance Use in Pregnancy and its Association with Cardiovascular Events. JACC Adv. 2023;2(8):100619.